Grangegorman and the treatment of soldiers' trauma
10 November 2022Downloads
Author Eamon Delaney leads the ‘The Lion and the Shamrock’ project which shares some of the legacy of military history of the north Dublin area, including Grangegorman. Here Eamon explores the treatment of soldiers with psychological trauma resulting from their experiences of the First World War at the Richmond War Hospital, a facility on the grounds of the then Richmond District Asylum located at Grangegorman.
The revitalised Grangegorman campus, with its many young and eager students, is an uplifting and poignant sight, given its historical role in the treatment of those mentally and physically challenged. Part of the Grangegorman legacy is often unheralded—its role in the treatment of soldiers suffering from trauma as a result of World War One. Just as wider mental challenges were often unexplored at the time, the soldiers’ trauma was then also relatively unacknowledged.
At the time, the trauma was known as ‘shell shock’; now it is more collectively referred to as PTSD—Post-traumatic Stress Disorder. Symptoms included disturbing flashbacks, nightmares, acute nervousness and exceptional and intense deliriums. Treatment focused on the effect of trench warfare and exposure to constant, high-explosive shelling. World War One was, after all, an intense, close-quarters conflict, involving a level of mechanised combat never before seen.

The European battlefront. Soldiers suffered more trauma because they were confined to trenches
and subject to constant shelling.(Courtesy of the Imperial War Museum, London)
Almost 200,000 Irishmen fought in World War One, an estimated 40,000 of whom were killed and many more wounded and psychologically damaged. The treatment of physical injury was obviously considerable and took place mainly in hospitals in Britain, but also in Ireland. In Dublin, physical care was provided to the war wounded in hospitals such as the Adelaide and in Drumcondra, and in the military care facilities at the King George V (now St Bricin’s Military Hospital) and Leopardstown Park hospitals. Patients suffering psychological trauma were treated at Richmond War Hospital, a facility on the grounds of the Richmond District Asylum located at Grangegorman. Between 1916 and 1919, it treated 368 patients, of whom about half were reported as having recovered following their treatment.
In the context of the number of killed and wounded, the contribution of Grangegorman in terms of those treated was numerically quite small. The treatment provided at the Richmond War Hospital was, however, vital and pioneering, and it contributed notably to the further development of this very important area of health care.

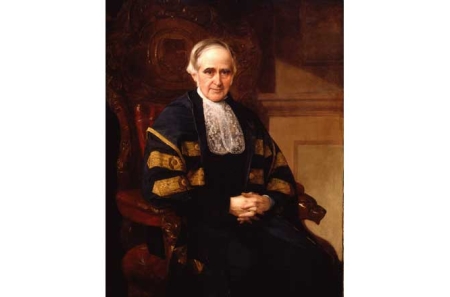
Sir Gordon Morgan Holmes, Dublin-born psychiatrist, who was a pioneer in
the treatment of shell shock.(Courtesy of the National Portrait Gallery, London)
The facility was overseen by Gordon Holmes, a pioneering British neurologist, originally from Dublin, who had worked in the war zone and whose efforts deepened the understanding of PTSD.[1] Holmes’s medical role in the army was an important one, for it was neurologists who initially attended the nervous patient—not psychiatrists, who worked in the asylums with the psychotic and organically impaired. This changed as the awareness of shell shock grew.
Despite the limitations on its resources, Richmond District Asylum, and the Richmond War Hospital, was regarded as ‘a generally forward-looking institution that pointed the way for future reform of Ireland’s asylum system and, along with the other war hospitals, brought significant changes to the practice of psychiatry’.[2] According to the Resident Medical Superintendent at Grangegorman, over half of the patients at Richmond War Hospital ‘were successfully treated and enabled to return to their homes without the blemish of having been certified insane’.
Obviously, in what was a more macho era, a certain stigma attached to PTSD, which probably added to the soldiers’ trauma. The army was also initially unwilling to acknowledge the impact of PTSD, for fear that it would demoralise the fighting troops. This official reluctance changed, however, with the prospect of having ‘disturbed’ soldiers ‘behind the lines’, creating instability, and so the soldiers were sent to facilities such as the Richmond War Hospital for treatment.
By today’s standards, the symptoms might seem predictable and entirely comprehensible; the case histories of soldiers admitted include descriptions of anxiety, fatigue, neuralgia, headache and depressed mood. There was also actual loss of speech or hearing, although treatment was applied to reverse these conditions. Hallucinations of sight and hearing were sometimes present, but most of the soldiers were quite conscious of the hallucinations, and realised that they were abnormal, and were, therefore, not to be regarded as ordinarily insane patients suffering from hallucinatory state.

A Royal Engineers tunnelling crew in World War One.
(Courtesy of the Imperial War Museum, London)
The treatments provided at the Richmond War Hospital might seem rudimentary and often primitive by modern standards, but they were a big step on from the existing treatment, which was effectively none, apart from what was ‘self-administered’ by the patient through the use of alcohol or hard physical exertion as an escape. War neurosis was regarded as attributable, at least in part, to unconscious psychological conflict in the soldier’s mind. Hospital treatments, therefore, were more psychological in tone.
As psychiatrist Brendan Kelly outlines in his 2015 article on shell shock, treatments included hypnosis and abreaction, which involved soldiers re-experiencing or re-living traumatic memories in an effort to purge them of their emotional impact.[3] In all cases there was a strong emphasis on prompt treatment, cognitive re-structuring of traumatic experiences (that is, thinking differently about the past) and collaboration with the therapist in the search for a cure.
Many of these therapies have certain similarities with current cognitive and behavioural approaches to PTSD, focusing on altering patterns of thought and behaviour in order to reduce symptoms. There were, however, other approaches to the management of shell shock that certain authorities viewed as being equally effective as—if not more effective than—approaches based on discipline, hypnosis, re-experiencing or abreaction. These included, most notably, approaches based primarily on rest and less intrusive forms of therapy.
One case reported on by Kelly recorded at the Richmond War Hospital involved Private VW, who had apparently been ‘blown out of a trench’ at the Battle of Arras in 1917, and since then ‘his speech has been affected’. Private VW’s ‘tongue [was] tremulous. Speech stammering and hesitating’. Mentally, he ‘has headache every now and again and suffers from noises in his head at times’, and he had also complained of ‘visions’ and ‘insomnia’.[4] Rest and treatment, however, had a positive effect. Later, Private VW ‘states he had no voices in his head since he came here and that he is feeling much better’. Two weeks later, Private VW was ‘bright and cheerful and is looking much stronger. He states he is feeling very much better’. This improvement was sustained, and one month after admission Private VW continued ‘to improve. He states he is now feeling all right in every way except that he is not physically strong. Sleeps and eats well’. Two months after admission, Private VW was ‘discharged and sent to his home’. [5]
Another case involved Lieutenant ST, a single, 19-year-old lieutenant admitted from the King George V Hospital. On admission, he had a cough and his ‘tongue and limbs are tremulous’. Mentally, Lieutenant ST was ‘dull and depressed and his memory is confused. He complains of pains and noises in his head and insomnia. He is unable to give a collected account of himself. He cannot give many particulars of his service. He, however, states that he served at Salonika and in France and came home suffering from shell shock’.[6]
On his first night at the Richmond War Hospital, Lieutenant ST ‘remained quiet and slept well during the night’. One week after admission, Lieutenant ST was ‘somewhat brighter and more cheerful but his memory is still confused’. Two weeks after admission, he was still ‘improving gradually. He states he is feeling much better and that his head is much less troublesome’. One week later, Lieutenant ST was ‘transferred to Belfast War Hospital’, which also dealt with soldiers for mental and psychological problems.[7]
After the war, the War Office’s committee of enquiry into shell shock addressed the issue of treatment in a comprehensive report (1922), drawing attention to the importance of rest in preventing shell shock in the first instance, including the need for frequent leave and immediate rest in cases showing initial symptoms of nervous breakdown. Morale depended chiefly on a sense of security and comfort, the report said. ‘Officers should be assiduous in their concern for their men. Removal from the front and visits home lessen the incidence of “shell-shock”’. In its final recommendations the committee warned against the indiscriminate use of therapies based on discipline, hypnosis, re-experiencing or abreaction. There was instead a strong emphasis on the curative properties of simple ‘rest of mind and body’.[8]

A soldier recuperates at Leopardstown Hospital in south Dublin, which also treated post-traumatic stress. (Courtesy of Leopardstown Hospital archive)
In this context, the treatment of PTSD at the Richmond War Hospital in Grangegorman was laudatory and humane. It was also consistent with the considerable help and assistance given by the British authorities to veterans, quite in contrast with the hands-off approach of the new Irish state. The concept of post-traumatic stress was then in its infancy, however, and veterans were expected to just ‘get on with it’, which, in fairness, many did, and it should be acknowledged that many veterans did resume their civilian lives without any apparent problems. But this was to mask what was going on below the surface.
In my own project, the Lion and the Shamrock, there is a section called Personal Stories, in which the descendants of soldiers from World War One are interviewed. A recurring finding is that veterans often simply didn’t talk about their war-time experiences, or referred to them obliquely for fear of reactivating the trauma. In other cases, they just drank and smoked incessantly afterwards, to deal with the impact. Or not ‘deal’ with it, more likely: an extraordinary amount of experience was bottled up, for understandable reasons. For many, however, the aftermath was an ongoing nightmare—literally so, for it was often at night that the worst anxieties occurred.[9]
This trauma added to what was already a difficult transition to civilian life for many Irish veterans, much more so than after other conflicts. This was because of a sense of waste about a long war which, by 1918, seemed pointless and unnecessary. Additionally in Ireland, the political landscape had completely changed after the 1916 Rising and with the prospect of Irish Independence, and veterans who had fought in the British army were officially shunned. The great political changes meant that, having been sent off on their military adventure like conquering heroes, they no longer felt welcome on returning home.

The Richmond War Hospital today; now part of the TU Dublin Grangeorman campus, and a gym for students. (Photo by the author)
It is to the great credit of the then authorities at Grangegorman that they engaged in treating the trauma experienced by soldiers of World War One. It is also consistent with the hospital’s long-term history in dealing with mental health, and with the military. Today, a small road adjoining Grangegorman at Rathdown Road is named Marne Villas, in remembrance of the great World War One battle and of the men who suffered there.
1 A.D. MacLeod, ‘Shell shock, Gordon Holmes and the Great War’, Journal of the Royal Society of Medicine 97 (2) (February 2004), 86–9.
[2] Brendan D. Kelly, ‘He lost himself completely’: shell shock and its treatment at Dublin’s Richmond War Hospital, 1916–1919’ (Dublin, 2014; Liffey Press).
[3] Brendan D. Kelly ‘Shell Shock in Ireland, The Richmond War Hospital, Dublin (1916-19)’, History of Psychiatry 2015, Vol. 26(1), 53
[4] Case-history drawn from: National Archives of Ireland (NAI), Richmond War Hospital Case Book (1918–1919), BR/PRIV 1223, Richmond War Hospital. The names, regiments, precise admission dates and other identifying details relating to the soldiers are not presented, in order to preserve anonymity.
[5] NAI, Richmond War Hospital Case Book (1918–1919).
[6] NAI, Richmond War Hospital Case Book (1918–1919).
[7] Kelly ‘Shell Shock in Ireland’, 51-52.
[8] British National Archives, UK War Office, WO 32/4748, Report of the Committee of Enquiry into Causation and Prevention of ‘Shell-Shock’ (1922); available online at: https://www.nationalarchives.gov.uk/education/resources/medicine-on-the-western-front-part-two/war-office-report-on-shell-shock/ (last accessed 26 October 2022).
[9] More details are available at the Personal Stories section of The Lion and the Shamrock: the legacy of history, families and the military project website. See, for example, the entry for ‘John Coyle—Chain smoking veteran who never spoke of war’, which can be accessed at: https://thelionandtheshamrock.com/2021/03/11/john-coyle-999999 (last accessed 26 October 2022).